Addis Ababa, Ethiopia, 27th November 2025
“A bold call for African Union Heads of State to commit to digitalizing at least 90% of Africa’s Primary Health Care systems, including community health systems, by 2035 as a cornerstone of Africa’s Health Security and Sovereignty (AHSS) Agenda.”
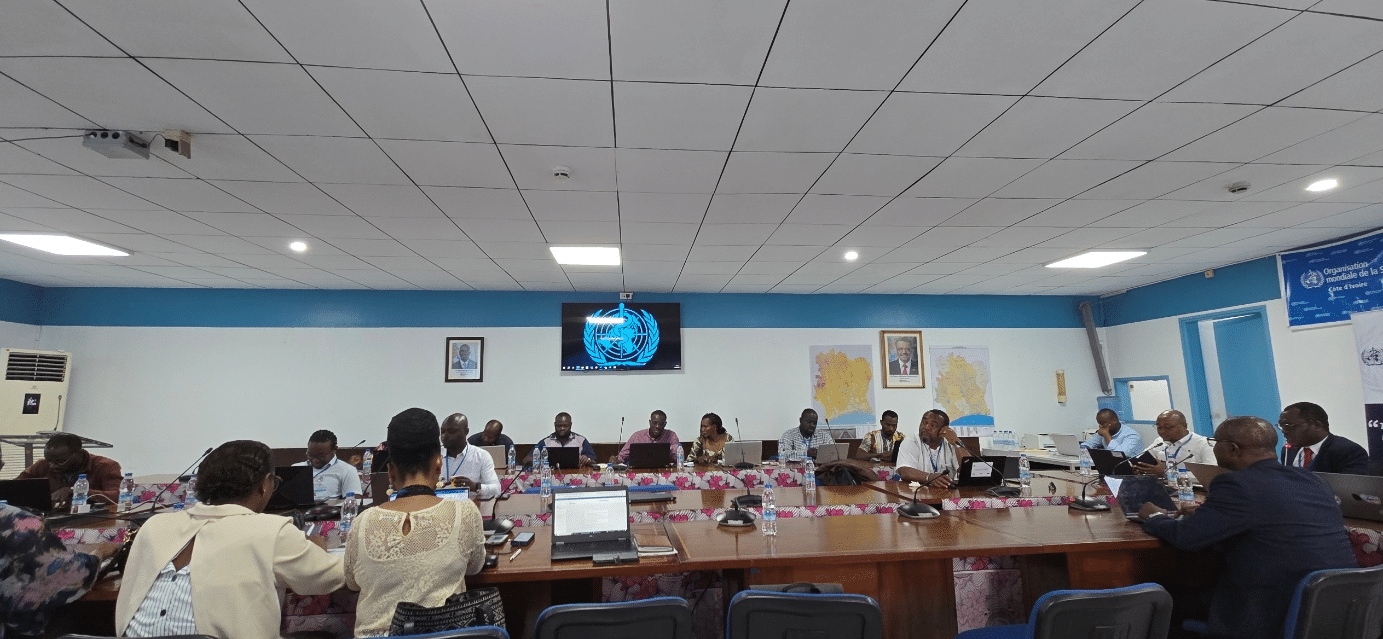
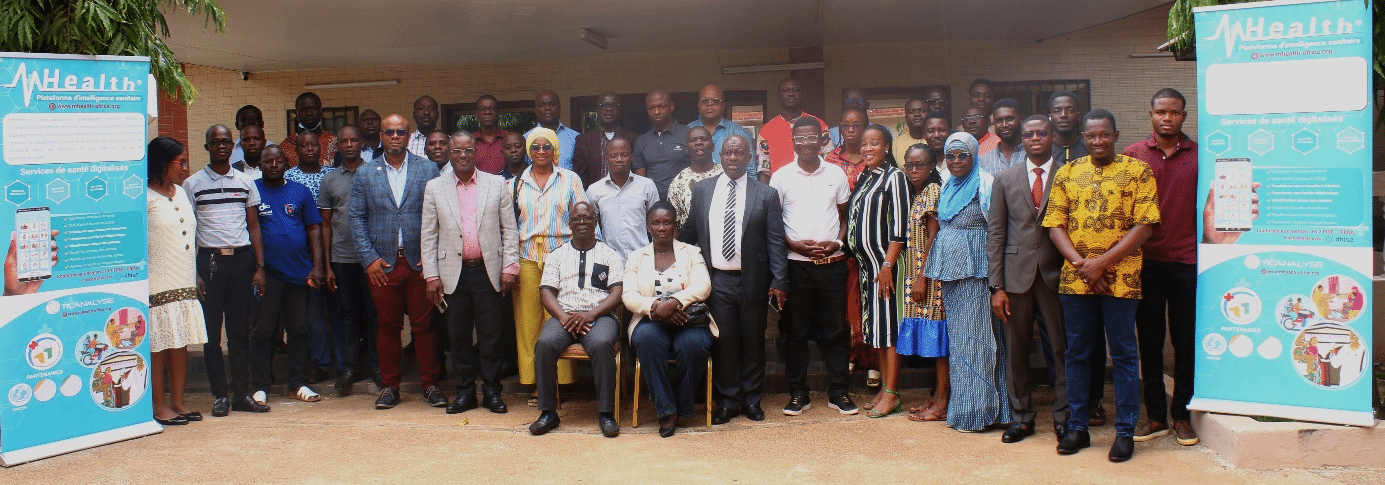
On November 26–27th, 2025, Africa CDC convened the PHC Digitalization Experts Committee (PHC-DEC) at its Headquarters in Addis Ababa, Ethiopia to initiate the development of the continental framework for a full digitalization of the Primary Health Care system. This outcome statement is submitted to Africa CDC leadership and issued as a political call to Heads of State and Government, and Africa’s partners, to position PHC digital transformation as a strategic and sovereign investment that accelerates the AHSS Agenda, the Lusaka Agenda’s five shifts, and the continent’s broader Agenda 2063 aspirations.
Africa stands at a defining moment characterized by a dual burden of communicable and non-communicable diseases, combined with climate pressures and socio-economic inequalities. Disease outbreaks have risen by over 41% between 2022 and 2024, while overseas development assistance (ODA) has declined by nearly 70% since 2021. The continent continues to import over 90% of essential health commodities and only 30% of its health systems are digitalized. This widening gap between rising health security threats and shrinking external financing underscores the urgency for Africa to build sovereign, digitally enabled, domestically financed systems that ensure preparedness, resilience, and accountability.
Primary healthcare is the frontline of the health system, where over 80% of health needs can be managed, yet it receives the least investment in most settings and is the least digitalized. The evidence from WHO and the World Bank on the benefit of digitalizing PHC is compelling; digitized community surveillance systems can detect outbreaks 7–21 days earlier, digitalized PHC facilities cut diagnostic delays by 30–50%, and for every USD 1 invested in digital transformation of PHC, countries can yield USD 6–10 through reduced mortality, lower treatment costs, and operational efficiencies. These gains translate directly into strengthened national security, improved fiscal space, and enhanced accountability, core tenets of the AHSS and Lusaka Agendas.
Digital transformation will catalyze investment in PHC and improve access and delivery of health services across the continuum of prevention and care, while enabling the continent to build a sovereign, resilient, data-driven PHC system that protects every woman, every child, and every community. There is economic benefit from a market estimated at at least USD 40 billion annually for Electronic Medical Records (EMR) alone, representing an unprecedented opportunity for African innovation, local manufacturing, and digital sovereignty.
There are promising examples across Africa where PHC digitalization has been implemented with positive impact on health systems resilience. For example, Rwanda has digitized more than 90% of its PHC system, enabling rapid outbreak alerts and significant reductions in maternal and newborn deaths.
Similar examples have been demonstrated in Egypt, Tunisia, Morocco, Rwanda, Kenya, Ethiopia, Ghana, South Africa, Burkina Faso, Niger and Côte d’Ivoire, where digital PHC platforms have been deployed. These countries illustrate that Africa’s rapidly maturing public health architecture is strongest when digital systems connect individuals to frontline workers, communities to facilities, and facilities to national and continental health intelligence hubs, creating the backbone of Africa’s PHC and health security intelligence ecosystem.
To fully realize these benefits, PHC digitalization must be socially accepted and trusted by the populations it is meant to serve. This requires structured communication and community engagement so that patients and communities understand, support, and benefit from digital tools, while being assured of the confidentiality and responsible use of their health data.
We, members of the PHC-DEC, support Africa CDC’s call under Africa’s Health Security and Sovereignty (AHSS) Agenda to leverage data and digital transformation as a key pillar. We therefore call for a future-defining continental commitment that positions PHC digitalization as a strategic lever for achieving AHSS, implementing the Lusaka Agenda’s five shifts, and accelerating progress toward universal health coverage under Agenda 2063.
Specifically, we urge the African Union Heads of State and Government to:
- Commit to the digitalization of at least 90% of Africa’s Primary Health Care systems by 2035, including community health systems and those in fragile, hard-to-reach, and conflict-affected settings, anchored in a set of minimum, continentally agreed digital health functionality standards that guarantee interoperability, equity, and data sovereignty.
- Champion the designation of “Digital Health Transformation for Africa” as the African Union Theme of the Year for 2027, to catalyze political momentum, mobilize domestic and continental financing, and ensure coherent partner alignment in support of the AHSS and Lusaka Agendas.
- Advocate for the establishment of a high-level Presidential Task Force on Primary Health Care Transformation to drive whole-of-government leadership, ensure accountability for delivery, and coordinate national and sub-national efforts toward a digitally enabled, people-centred PHC system.
Thank you.
Endorsed by the Members of the Africa CDC Primary Health Care Digitalization Experts Committee on November 27th, 2025 in Addis Ababa.